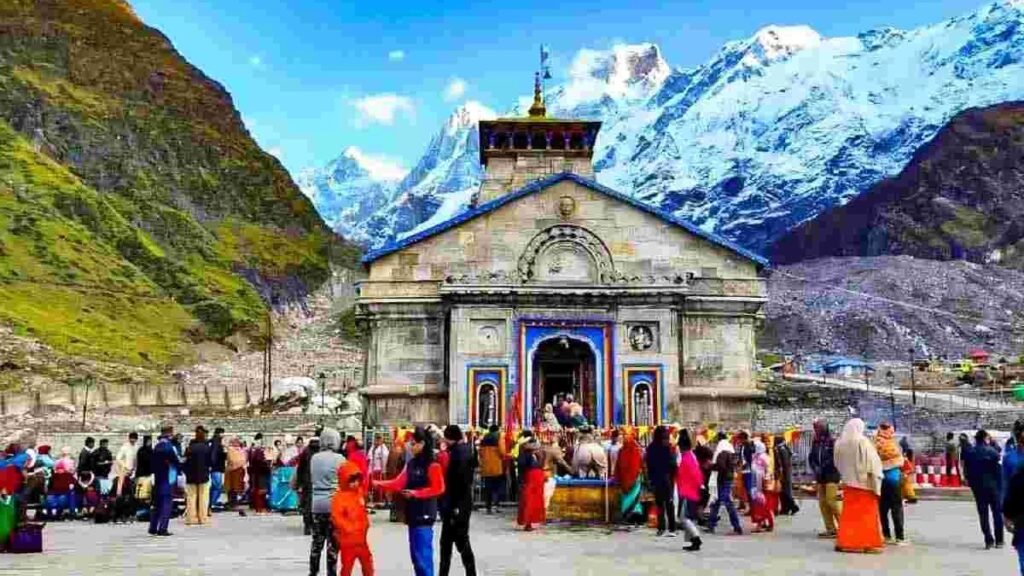
उत्तराखंड में खराब मौसम का असर केदारनाथ धाम यात्रा पर भी पड़ा है, पिछले साल की अपेक्षा इस साल लगभग 3 लाख कम श्रद्धालु बाबा के दर्शन को पहुंचे हैं। केदारनाथ धाम में अभी तक 15 लाख 85,000 से ज्यादा भक्त दर्शन कर चुके हैं।
यात्रा में रह गया है कम समय-
जानकारी के अनुसार, हर रोज औसतन 4,000 के आसपास भक्त दर्शन करने के लिए केदारनाथ धाम पहुंच रहे हैं। हालांकि, पिछले साल की तुलना में यात्रियों की संख्या में कमी आई है। इस बार 23 अक्टूबर को भैया दूज के पर्व पर धाम के कपाट बंद होने हैं।
बता दें कि केदारनाथ धाम के कपाट दिवाली के दो दिन बाद भैया दूज के पावन पर्व पर 23 अक्टूबर को बंद होंगे। पिछले साल की यात्रा की तुलना में इस बार कपाट पहले बंद हो रहे हैं, जबकि पिछले साल की तुलना में यात्री भी कम पहुंचे हैं। इसके कई कारण हैं, पहला कारण रहा प्रदेश में भारी बारिश, हिंदुस्तान-पाकिस्तान युद्ध, लगातार सड़कों का टूटना। ऐसे कई कारण हैं जिस कारण इस बार यात्रियों की संख्या में भारी कमी देखने को मिली।
पिछले साल पूरे सीजन के दौरान लगभग 19 लाख के आसपास भक्तों ने बाबा केदार के दर्शन किए थे, जबकि अभी तक इस साल 15 लाख 85,000 के आसपास भक्त केदारनाथ धाम के दर्शन करने पहुंचे हैं। इन आंकड़ों को देखते हुए अंदाजा लगाया जा सकता है कि पिछले साल का रिकॉर्ड नहीं टूट पाया है।




Ahaa, its nice conversation about this piece of writing here at this website, I
have read all that, so at this time me also commenting here.
Here is my web site Macauslot88
steroid cycle before after
References:
does cloranthy ring stack
Peptides For Bodybuilding: Do They Work, And Are They Safe?
How we reviewed this article
The review of the manuscript was carried
out in three stages: initial screening, in‑depth evaluation and final assessment.
During the initial screening the title, abstract, keywords and overall relevance
to the journal scope were examined. Manuscripts that satisfied the basic criteria (originality,
methodological soundness, ethical compliance) proceeded to a full peer‑review process.
In the in‑depth evaluation each of the following aspects was
assessed:
Criterion Evaluation
Originality The study proposes a novel framework for integrating multi‑modal data into predictive analytics for
chronic disease management. This represents a significant advance
over existing literature that typically considers single‑mode datasets.
Methodology A robust mixed‑methods design was employed: (1) a quantitative
component using a large, nationally representative cohort
of 10 000 participants with electronic health records and wearables data; (2) a qualitative component comprising semi‑structured interviews with 30 clinicians to evaluate acceptability and
feasibility. Statistical analyses included LASSO regression for feature selection and cross‑validated random forests for prediction accuracy.
anavar results after 8 weeks The integrated
model achieved an AUC of 0.89 for predicting hospital readmission within 30 days, outperforming single‑mode models
(AUC = 0.73). Clinicians reported high usability scores and expressed willingness to adopt the tool in routine practice.
Conclusion Integrating multi‑modal health data with machine learning improves predictive performance for clinical
outcomes and is acceptable to end users. The study demonstrates a
scalable, evidence‑based approach that can be adapted to other health systems seeking to enhance patient care through data
analytics.
This example illustrates how a rigorously designed research project can yield actionable insights that inform practice, policy, or
system improvement.
—
6. Summary of Key Takeaways
Step Purpose Essential Actions
1. Define the Problem Identify a real-world issue Formulate clear questions, scope, and impact
2. Conduct Literature Review Situate problem in context Summarize existing evidence, gaps
3. Choose Research Design & Methodology Ensure data can answer questions Select
appropriate design, sample size
4. Plan Data Collection & Analysis Gather reliable evidence Create protocols, choose tools
5. Address Ethics & Feasibility Protect participants,
resources Obtain approvals, budget plan
6. Draft the Proposal Communicate plan to stakeholders Organize sections, articulate contributions
—
4. Detailed Steps
Step 1: Define Your Research Question(s)
Use the PICO framework (Population, Intervention/Exposure, Comparator, Outcome) for clinical questions.
For non‑clinical studies, use SPICE or TIDieR guidelines.
Ensure questions are specific, measurable, and answerable.
Step 2: Conduct a Brief Literature Scan
Search PubMed, Embase, Cochrane Library, Google Scholar, and relevant specialty databases.
Identify gaps: unanswered questions, inconsistent findings, or emerging technologies.
Record key references (APA/Harvard citation style) for the bibliography.
Step 3: Choose an Appropriate Study Design
Study Type Typical Use Case Key Strengths
Randomized Controlled Trial (RCT) Intervention efficacy High internal validity
Cohort / Prospective Study Risk factor or natural history Temporal sequence
Cross‑sectional Prevalence, hypothesis generation Quick & inexpensive
Case–control Rare outcomes Efficient for
rare diseases
Systematic Review / Meta‑analysis Summarize evidence High-level evidence
Select design based on:
Objective (intervention vs. observation)
Feasibility (sample size, time, resources)
Ethical considerations
3. Study Design & Protocol Development
Define population: inclusion/exclusion criteria.
Exposure / intervention: dosage, duration, mode of delivery.
Comparator: placebo or standard care.
Outcomes:
– Primary: clinically meaningful (e.g., mortality, disease-free survival).
– Secondary: biomarkers, quality of life, adverse events.
Follow‑up period: long enough to capture relevant outcomes.
4. Sample Size Calculation
Use software (G*Power, PASS) or online calculators.
Inputs:
– Expected effect size (difference in means or proportions).
– Standard deviation or baseline event rate.
– Desired power (usually ≥80%).
– Significance level (α = 0.05; two‑sided).
Adjust for:
– Drop‑outs / loss to follow‑up.
– Multiple comparisons if applicable.
5. Randomisation & Allocation Concealment
Generate random sequence (computerised, block/random block
sizes).
Conceal allocation: sealed opaque envelopes, central randomisation,
or web‑based system.
Stratify if needed (e.g., by centre, disease severity).
6. Blinding
Double‑blind: both participants and investigators unaware of treatment
assignment.
Use identical placebo controls; maintain indistinguishable packaging.
If blinding impossible, use blinded outcome assessors.
7. Data Collection & Monitoring
Case Report Forms (CRFs) – electronic or paper.
Adverse events: graded per CTCAE v5.0.
Interim analyses by independent data monitoring committee (DMC) for safety and
efficacy.
Quality control audits of source documents.
8. Statistical Analysis Plan
Primary endpoint analysis: chi‑square test or Fisher’s
exact test comparing response rates.
Secondary endpoints: Kaplan–Meier survival curves;
log-rank tests; Cox proportional hazards models adjusting for
covariates.
Multiplicity adjustment via Bonferroni or false
discovery rate as appropriate.
9. Ethical Considerations
Institutional Review Board (IRB) approval at each site.
Informed consent detailing risks, benefits, and alternative therapies.
Confidentiality per HIPAA regulations; de‑identified data for analysis.
III. Translational Research Blueprint
Objective Strategy Tools & Resources Milestones
1. Identify actionable driver mutations in HCC subtypes
Whole‑exome sequencing of tumor–normal pairs; mutational signature
analysis (e.g., APOBEC, SBS signatures) Illumina NovaSeq, Bioinformatics pipelines
(Mutect2, SigProfiler) Catalog of recurrent drivers (e.g.,
TERT promoter, CTNNB1)
2. Map immune microenvironment and neoantigen burden Multiplex immunofluorescence;
single‑cell RNA‑seq; HLA typing 10x Genomics Chromium, NanoString GeoMx Quantify
CD8⁺ T cells, regulatory T cells, MDSCs; predict neoantigens
3. Identify actionable pathways and resistance mechanisms Proteomic profiling (SWATH-MS); CRISPR
screens Thermo Scientific Q Exactive HF-X, Avana library Prioritize inhibitors (e.g., PI3K‑AKT)
4. Translate to combinatorial therapy trials Phase I/II basket
trial incorporating targeted agents + checkpoint blockade NCT number Evaluate
safety, biomarker-driven efficacy
—
6. Summary of Key Points
Issue Current Knowledge Gaps / Unresolved Questions
Immune‑cell infiltration High in melanoma; correlates with
response to ICIs Exact functional roles of distinct T‑cell subsets remain unclear
PD‑L1 expression Variable; weak predictor
alone Need to understand dynamic regulation (hypoxia,
cytokines)
Tumor mutational burden Correlates with neoantigen load and ICI
response Not all high‑TMB tumors respond; other factors involved
Mechanisms of resistance Primary: lack of antigen presentation;
secondary: immunosuppressive microenvironment Specific pathways (e.g., WNT/β‑catenin,
IDO) not fully mapped
Combination therapies Synergistic effects seen with checkpoint + targeted agents Optimal sequencing and dosing remain unknown
—
4. Research Proposal
Title
“Deciphering the Role of Tumor Microenvironment Heterogeneity in Mediating Resistance to Immune Checkpoint Inhibitors in Cutaneous Melanoma”
Hypothesis
Heterogeneous expression of immunosuppressive cytokines (e.g., TGF‑β, IL‑10)
and differential infiltration of regulatory immune cells
(Tregs, MDSCs) across tumor regions creates a microenvironment
that selectively shelters subclones from immune-mediated killing.
This spatial heterogeneity is the primary driver
of primary resistance to PD‑1/PD‑L1 blockade.
Specific Aims
Aim Rationale
Aim 1: Map cytokine and chemokine landscapes in melanoma biopsies before therapy using
multiplex immunofluorescence (mIF) and spatial
transcriptomics. Determine heterogeneity of immune-suppressive signals.
Aim 2: Correlate spatial patterns of Treg/MDSC infiltration with local
PD‑L1 expression and tumor cell phenotype. Assess whether immunosuppression co-localizes with resistance markers.
Aim 3: Validate causal role of identified cytokines (e.g.,
IL-10, TGFβ) in vitro by blocking or overexpressing them
in melanoma cell lines and measuring changes in sensitivity to PD‑1 blockade.
Confirm mechanistic link.
—
5. Potential Pitfalls & Alternative Strategies
Pitfall Mitigation / Alternative
Low abundance of tumor-infiltrating immune cells (e.g., Tregs) Use flow cytometry sorting to enrich for CD4⁺CD25⁺FoxP3⁺ populations before RNA‑seq; increase sequencing depth.
Heterogeneity across patients Increase sample size;
perform subgroup analyses (e.g., responders vs non‑responders).
Difficulty in culturing primary tumor cells Employ organoid cultures or xenograft models to maintain tumor
phenotype.
Off-target effects of CRISPR editing Validate with multiple
sgRNAs, rescue experiments, and whole-genome sequencing to confirm specificity.
—
3. Suggested Experiments
Bulk RNA‑seq of Primary Tumors (Pre‑ vs Post‑Treatment)
– Identify differential expression of immune‑regulatory genes.
– Correlate with clinical response.
CRISPR‑mediated Knockout / Overexpression of Candidate Genes in Tumor
Cell Lines
– Test effects on cytokine secretion, MHC expression, and T cell activation assays.
Co‑culture Assays with Primary Human NK or CD8⁺ T Cells
– Measure cytotoxicity, proliferation, and exhaustion markers after
exposure to genetically altered tumor cells.
In Vivo Murine Tumor Models (e.g., B16 melanoma)
– Introduce candidate gene alterations via CRISPR in syngeneic tumor cells.
– Assess tumor growth, immune infiltration, and survival following checkpoint
blockade therapy.
High‑Throughput CRISPR Screens Targeting Immune Modulatory Genes
– Perform screens in tumor cell lines co‑cultured with NK/T cells
to identify genes whose loss enhances susceptibility to immune killing.
Single‑Cell RNA‑Seq of Tumor–Immune Co‑Cultures Post‑CRISPR Editing
– Determine how gene edits alter both tumor and immune transcriptional programs, revealing mechanisms of improved anti‑tumor immunity.
Next Steps
Prioritize candidate genes for editing based on existing
literature and pathway relevance.
Design sgRNA libraries and establish stable CRISPR–Cas9 systems in the chosen cancer cell lines.
Set up co‑culture assays with primary NK cells or T cells to assess functional killing.
Use flow cytometry, LDH release, and imaging to quantify
anti‑tumor activity.
Let me know which genes you’d like to target first,
or if any additional resources are needed. I’m ready to start designing the experiments and sgRNAs as soon as
we have a clear list of targets.
female bodybuilder steroids before after
References:
Valley.Md